A bariatric endoscopy procedure can do more than just help patients lose weight
A bariatric endoscopy procedure has a range of benefits, although many people only associate this new technique with weight loss as it can be a great option for those looking to lose weight without surgery. However, this form of treatment can also be of benefit to those who have put on weight following traditional bariatric surgery, while it also reduces the likelihood of complications occurring after such a procedure.
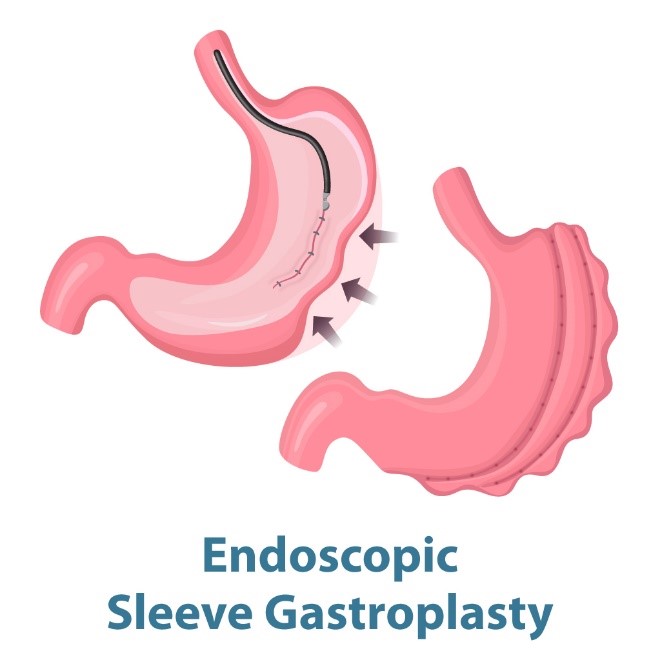
Endoscopic Sleeve Gastroplasty (ESG)
This procedure relies on similar principles to a sleeve gastrectomy but differs in that it folds and stitches the stomach in on itself using an endoscopic device called OverStitch
TM. This involves the doctor inserting the device in through the mouth instead of making an incision in the abdomen. This reduces the risk of complications occurring, such as
GERD, leaks, stenosis, and infection. However, it does take a longer time to achieve the desired weight loss.
When compared to other similar procedures, such as an intragastric balloon, an endoscopic sleeve gastroplasty procedure has a significantly reduced risk of complications occurring (such as nausea, vomiting, and vomiting blood). In addition, the weight loss is achieved to a greater degree and lasts longer, too. Alternatively, when compared with aspiration therapy, which is no longer a preferred method of endoscopic procedure, an endoscopic sleeve gastroplasty carries a much lower risk of infection as there are no incisions made in the abdomen. As such, patients are not as inconvenienced by the procedure itself. However, both procedures take approximately 12 months for the desired weight loss to be achieved.
Bariatric endoscopy for revision of weight regain following bariatric surgery
Patients who regain the weight they lost after a Roux-en-Y gastric bypass or laparoscopic sleeve gastrectomy (LSG) may be considered for a bariatric endoscopy if they have gained up to 15% of the weight they lost in the first instance. Indeed, the procedure may be necessary in patients who are unsuitable for open forms of surgery, such as those who have developed a severe abdominal membrane called adhesions.
- Endoscopic sleeve gastroplasty for revision of a LSG: Should the patient’s stomach have enlarged in size from the size of a banana to the size of a rugby ball and medical staff have deemed that patient to be unsuitable for open forms of surgery, they may consider turning to an endoscopic sleeve gastroplasty procedure (ESG sleeve, as a revision, inside prior LSG sleeve). This involves an endoscopic device containing a tiny camera being inserted into the stomach. With this procedure, the OverStitchTM equipment can be used to fold and stitch the stomach in on itself to reduce its capacity.
- Endoscopic techniques for revision of a Roux-en-Y gastric bypass: A gastric bypass involves surgeons separating the stomach into two compartments. The first, smaller section (gastric pouch) is then responsible for receiving food from the esophagus and transferring it directly into the small intestine. This means that food can no longer enter the other section (excluded stomach). Should either the gastric pouch or the section connecting the gastric pouch to the small intestine expand, it will result in the patient being able to consume more and gaining weight.
-
Surgeons can stitch the gastric pouch to reduce its size and/or decrease the size of the section connecting it to the small intestine using the following techniques:
- The argon plasma coagulation technique: This involves an electrocautery device that destroys healthy tissue located in the gastric pouch as well as in the section connecting it to the small intestine. This then stimulates the growth of new tissue that results in a restricted gap for food to pass through, thus reducing the size of the connection between the gastric pouch and the small intestine.
- Endoscopic transoral gastric outlet reduction (TORe): This procedure involves two vital steps. First, argon plasma coagulation is performed, and then the surgeon will stitch the gastric pouch to the small intestine using an OverStitchTM device that is inserted through the patient’s mouth. This device acts like a sewing machine, stitching the gastric pouch to the small intestine in such a way that only a small outlet is left for food to travel through. This is why this is sometimes referred to as the ‘purse string’ technique.
Management of complications resulting from bariatric surgery
There are several complications that can arise from sleeve gastrectomy and Roux-en-Y gastric bypass procedures. However, bariatric endoscopy can provide a solution for those issues, as follows:
- Marginal ulcers: These tend to be present in the section connecting the gastric pouch to the small intestine and, in cases that are not receptive to antacid treatment alone, medical staff may perform an endoscopic full thickness closure of the ulcers to connect healthy sections of tissue surrounding the ulcers to one another.
- Gastrogastric fistula: This issue can lead to food flowing directly from the newly formed gastric pouch into the excluded stomach, which can result in additional nutrients being absorbed by the body and patients gaining weight. Such a problem can occur in patients who have undergone a Roux-en-Y gastric bypass. Medical staff can solve this problem by performing an argon plasma coagulation procedure to constrict the flow of food from the gastric pouch to the excluded stomach to former levels. Alternatively, a large clip may be fastened into place to close the opening so that the two sections are no longer connected. Fortunately, either procedure can now be performed endoscopically with no need for any incisions whatsoever.
- Leaks: Treatment depends on the size and length of time the leak has been happening, as well as any other underlying conditions the patient may have. The medical team consisting of surgeons and gastroenterologists, therefore, plays a crucial role in determining which treatment should take place, with some cases suitable for an endoscopic closure procedure.
- Stenosis: Medical staff are able to enlarge the affected section using a balloon dilator and/or a stent that must be inflated/placed to the appropriate size, so that unwanted weight gain does not occur thereafter.
- Gallstones: Removing gallstones from patients who have previously undergone a Roux-en-Y gastric bypass procedure is extremely complex due to the bile duct opening being in such close proximity to the small intestine and excluded stomach, while also at a considerable distance from the gastric pouch. Fortunately, medical staff are now able to reconnect the excluded stomach with the gastric pouch using an endoscopic procedure. This then enables the removal of stones from the bile duct via the small intestine, without an incision on the abdominal wall. After this has been performed, medical staff can close off the connection once more to avoid unwanted weight gain in the patient.
Here at Bumrungrad International Hospital, we work effectively as a team to ensure the highest levels of safety are maintained, while retaining a focus on achieving the best possible results for our patients. Our comprehensively assembled medical team consists of surgeons specializing in bariatric surgery procedures, experts in the field of bariatric endoscopy, and a highly experienced group of interdisciplinarians on hand to provide outstanding care for our patients. All of this means we are able to perform successful treatments and complicated revisions to existing issues.
Digestive Disease (GI) and Liver Center
2nd Floor, Building B, Bumrungrad International Hospital.
Please make an appointment by calling 02 011 2167-8
Open Sunday – Friday from 08:00 – 20:00
Open Saturday from 08:00 – 19:00
For more information please contact:
Last modify: May 05, 2025