Robotic–assisted da Vinci Surgery or Da Vinci® Prostatectomy or Robotic Prostatectomy is one of the most minimally invasive option available. Through high definition cameras, a very clear close-up view of the treatment area is available to the surgeon. The robotic arms mimic arm and wrist movements of the human operator, allowing for accurate and intuitive operation by the surgeon. Another equally vital treatment is brachytherapy, which involves planting a radiation-emitting element directly into the cancerous tumor via a tiny tube. The cancerous tissue will receive a high dose of radiation directly, while minimizing the level of radiation to the surrounding anatomy.
The prostate gland is a vital part of the male reproductive system. It is unique in that it does not stop growing when a man reaches adulthood, but continues to grow indefinitely. However, problems can occur when the prostate grows too big. In cases of simple prostate enlargement (benign prostate hyperplasia), symptoms such as painful or too frequent urination may be a mere annoyance. But if prostate cancer – the second most common form of cancer in men – is present, this is an altogether more serious situation. Statistics also show that prostate cancer is most often diagnosed in the advanced stages, which tends to complicate treatment.
Speedy diagnosis contributes greatly to successful treatment. The American Cancer Society recommends that men of certain ages have their blood tested for PSA levels annually. To better understand PSA screening, and what PSA test results mean, we sought the expertise of Dr. Charuspong Dissaranan, a urosurgeon at the Bumrungrad International’s Urology Center.
What is the purpose of PSA screening, and what do the results mean?
Dr. Charuspong: We use PSA screening to check for a protein that can indicate the presence of prostate cancer. Prostate cancer doesn’t usually produce physical symptoms in its earlier stages, but it does tend to raise PSA level. PSA screening provides a non-invasive method for measuring an important indicator of prostate cancer. However, the PSA levels alone doesn’t determine whether cancer is present or not.
.png)
How often should men go for PSA screening?
Dr. Charuspong: “It is recommended for men 50 and older to be tested once a year. If results are above normal range, your doctor may suggest a screening every six months as a way to monitor any possible changes and nip the cancer in the bud.”
What should I do next if my PSA level is high?
Dr. Charuspong: “The test result is usually available within two hours. If the PSA level is high, I would probably recommend an MRI, which scans the prostate and surrounding areas to create a detailed image. If the MRI confirms an abnormality, the likeliest next step is to perform an MRI ultrasound fusion biopsy to obtain tissue samples that will then be tested for the presence of cancer cells.
After the screening has been explained, the next question is of course the treatment. The treatment options – which often involve radiotherapy, chemotherapy, or hormone therapy – will depend on the stage or progression of the cancer. But at present, surgery to remove the prostate gland (prostatectomy) remains the most effective treatment for prostate cancer. The most favored surgical technique involves laparoscopic radical prostatectomy. With this method, the doctor inserts a tiny camera on a long thin tube (laparoscope) and performs the surgery with miniaturized tools via the images viewed on a monitor. The patient usually spends around three days recovering at the hospital after this kind of surgery.
But a newer and even more effective surgical technique is now available; Robotic–assisted da Vinci Surgery or Robotic Prostatectomy. Dr. Teerapon Amornvesukit, a urosurgeon at Bumrungrad International Hospital with many years of experience treating patients with prostate cancer, explains that the system’s 3D imaging helps surgeons to operate with far greater precision and accuracy when compared to open or standard keyhole (non-robotic) laparoscopic surgery.
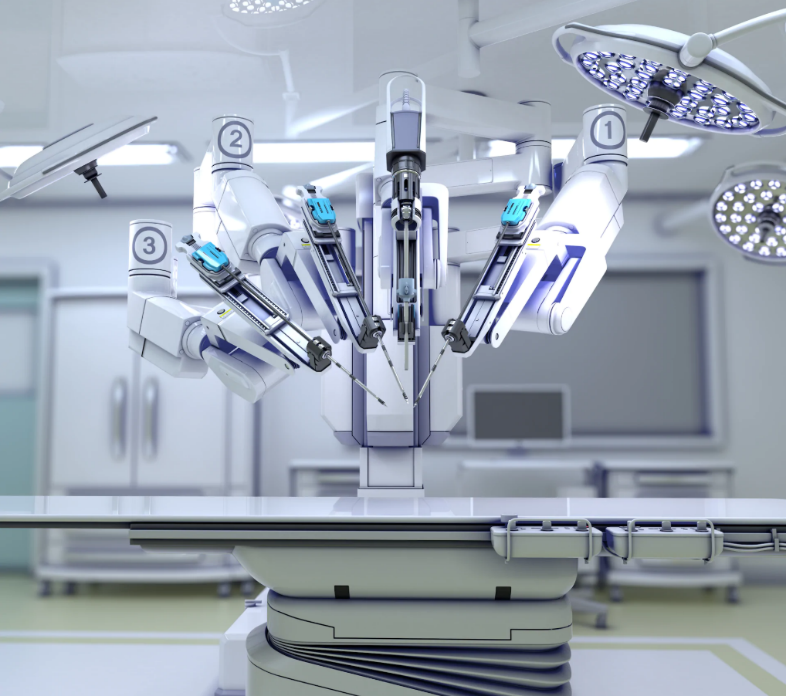 Through high definition goggles, a very clear close-up view of the treatment area is available to the surgeon. The robotic arms – which bear miniature surgical tools – mimic arm and wrist movements of the human operator with even greater range of motion, allowing for accurate and intuitive operation by the surgeon.
Through high definition goggles, a very clear close-up view of the treatment area is available to the surgeon. The robotic arms – which bear miniature surgical tools – mimic arm and wrist movements of the human operator with even greater range of motion, allowing for accurate and intuitive operation by the surgeon. This not only has the advantages of less pain and faster recovery time, as is the case with laparoscopic surgery, but also reduces the chances of urinary incontinence or erectile dysfunction post-surgery.
 Another equally vital treatment is brachytherapy, which involves planting a radiation-emitting element directly into the cancerous tumor via a tiny tube. The cancerous tissue will receive a high dose of radiation directly, while minimizing the level of radiation to the surrounding anatomy. Dr. Apichart Panichevaluk
Another equally vital treatment is brachytherapy, which involves planting a radiation-emitting element directly into the cancerous tumor via a tiny tube. The cancerous tissue will receive a high dose of radiation directly, while minimizing the level of radiation to the surrounding anatomy. Dr. Apichart Panichevaluk, an expert in radiology and radiation therapy at the
Horizon Cancer Center, explains further:
“
In high dose rate (HDR) brachytherapy, we insert a tiny needles right into the prostate using a
Transrectal Ultrasound Guidance (TRUS) before a pre-calculated dose of radiation is released into the cancerous tissue. When this is done, the apparatus is removed, leaving nothing behind. The advantage is that the radiation levels can be continuously adjusted while the tube is still inside the patient. HDR combined with external beam radiation therapy is very effective against medium to high-risk localized prostate cancer with success rate of over 90%, whereas the side effects are considerably less when compared to other approaches.
.jpg) For low-risk localized prostate cancer, permanent implantation is the preferred brachytherapy option.
For low-risk localized prostate cancer, permanent implantation is the preferred brachytherapy option. Here, the radiation source is implanted into the tumor permanently. The radiation source will about the size of a sesame seed, and slowly releases very small amount of low-level radiation until depleted.
Since the radiation source will sit permanently within the cancerous tumor until the radiation is depleted, precise calculation of the radiation dose is absolutely crucial.”
.png) There is even more option still. Image guided radiotherapy (IGRT), an upgraded version of the traditional external beam radiation therapy, could give the low-risk prostate cancer patients more than 90 percent cure rate. First, gold fiducial markers—three tiny grains of pure gold—are inserted into the prostate. The patient is then given a dose of radiation by a machine that is also able to perform a CT-scan. The three dense grains of gold will show up in the imagery, helping the physician to precisely target the tumor. This lessens the damages to the surrounding healthy tissue, as well as shortening the course of treatment greatly in comparison to previous modes of treatment.
There is even more option still. Image guided radiotherapy (IGRT), an upgraded version of the traditional external beam radiation therapy, could give the low-risk prostate cancer patients more than 90 percent cure rate. First, gold fiducial markers—three tiny grains of pure gold—are inserted into the prostate. The patient is then given a dose of radiation by a machine that is also able to perform a CT-scan. The three dense grains of gold will show up in the imagery, helping the physician to precisely target the tumor. This lessens the damages to the surrounding healthy tissue, as well as shortening the course of treatment greatly in comparison to previous modes of treatment.
The physicians at the Horizon Regional Cancer Center together with Urology Center and Robotic Surgery Center will take into account the size, location, and stage of the cancerous tumor as the determining factors in the patient treatment plan. Staying informed, aware, and regularly receiving check-ups is the way to be ready for anything.
Today, the knowledge and skill of the specialist physicians, combined with the most cutting-edge technology, makes prostate cancer a considerably less scary prospect than it used to be.
For more information please contact:
Last modify: April 30, 2025