What Is a Gastrostomy Tube and Why Is It Needed?
For some patients, eating and swallowing become difficult due to medical conditions such as
stroke, neurological disorders, or head and neck cancers. When regular food intake is insufficient, a
gastrostomy tube (G-tube) provides essential nutrition directly into the stomach. This is known as
enteral nutrition, a safe and effective way to maintain proper nourishment.
A G-tube is recommended for patients who:
- Have difficulty swallowing (dysphagia) and are at risk of choking.
- Cannot consume enough calories due to a medical condition.
- Require long-term nutritional support while recovering from surgery or illness.
- Have neurological conditions that impair swallowing.
Latest Guidelines on PEG Tube Placement
The American Society for Gastrointestinal Endoscopy (ASGE) has released updated guidelines for percutaneous endoscopic gastrostomy (PEG) tube placement. Developed by experts from institutions such as Johns Hopkins University, Harvard Medical School, and the University of Michigan, these recommendations ensure best practices for G-tube placement, management, and patient care.
How Is a Gastrostomy Tube Placed?
There are two main methods for inserting a feeding tube:
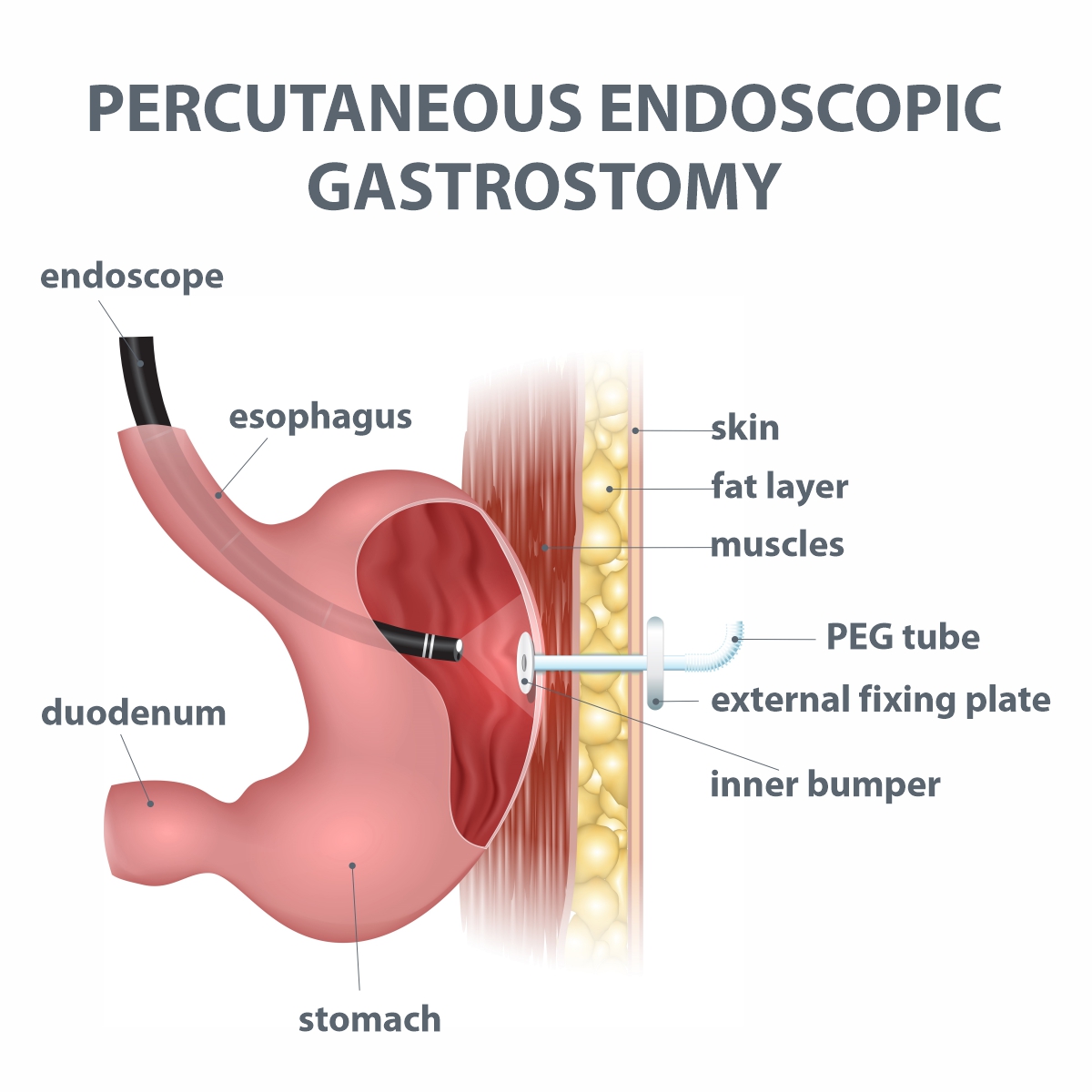
- Percutaneous Endoscopic Gastrostomy (PEG) – The Preferred Method
- A flexible camera (endoscope) is inserted through the mouth into the stomach.
- A small incision is made on the abdomen to guide the feeding tube into place.
- Performed under moderate sedation or anesthesia.
- Quick, safe, and effective; no need for X-ray guidance.
.jpg)
- Image-Guided Radiologic Gastrostomy (IR-G)
- Uses X-ray guidance with a contrast dye.
- Requires minimal sedation and a nasogastric tube for positioning.
- Preferred for certain patients with complex anatomical conditions.
Managing Medications Before and After PEG Placement
Patients may need adjustments to medications before PEG to reduce bleeding risks:
- Antiplatelet drugs (Aspirin, Clopidogrel, etc.) – ASGE recommends not stopping these medications, as they help prevent strokes and heart attacks.
- Anticoagulant drugs (Warfarin, Apixaban, etc.) – The decision to continue or pause these depends on bleeding risk and should be evaluated by a provider prescribing the medication.
How Soon Can You Start Tube Feeding After PEG?
Traditionally, doctors delayed feeding after PEG placement. However, new research suggests feeding can begin within 4 hours of the procedure, improving recovery time and overall health outcomes.
Special Considerations for Cancer Patients
Patients with malignant dysphagia (difficulty swallowing due to cancer) may require special PEG techniques to reduce complications like tumor seeding (cancer cell spread). The ASGE recommends:
- Traditional PEG (pull method) or
- Direct percutaneous gastrostomy (avoiding the oral cavity) based on the patient's condition.
Challenges and Future Research in PEG Management
While PEG is widely used, challenges remain:
- Placement in Patients with Altered Anatomy – More research is needed for those with prior stomach surgeries.
- Choosing the Right Tube Type – Various tube designs exist (e.g., low-profile tubes, retention balloons), but the best choice varies per patient.
- When to Replace PEG Tubes – No universal guidelines exist, requiring further study.
- PEG Safety in Patients with Ascites – Patients with fluid buildup in the abdomen face higher risks, requiring better safety strategies.
- Cancer Spread Risk with PEG – Research is ongoing to assess alternative methods to reduce metastasis.
- Managing Long-Term Complications – Issues like leakage, infections, and persistent fistulas need better-defined treatment strategies.
- Alternative Feeding Options – Some patients may benefit from jejunal (small intestine) feeding instead of gastric feeding, but further studies are needed.
Key Takeaways
- PEG is the preferred method for long-term feeding when normal eating is not possible.
- Stopping antiplatelet medications is not recommended before PEG placement.
- Feeding can begin within 4 hours after PEG insertion.
- Special techniques may be required for cancer patients to prevent complications.
- Ongoing research aims to improve PEG placement, management, and patient outcomes.
If you or a loved one requires a feeding tube, consulting a gastroenterology specialist is essential to determine the best approach for long-term nutrition and care.
Tossapol Kerdsirichairat, MD, FACG, FASGE
Clinical Associate Professor of Medicine
Advanced/Bariatric Endoscopy, Digestive Disease Center
Bumrungrad International Hospital
For more information please contact:
Last modify: March 31, 2025